On a concrete platform set into a steep hill in a Freetown slum, Daddy Hassan Kamara points to the tin-roofed shack behind him. “I was living here with my father, mother, wife, brothers,” he says. “I lost all my relatives inside a month.”
Ten years ago, the Ebola virus tore through west Africa, killing more than 11,000 people, including nearly 4,000 in Sierra Leone – around 40% of those infected in the country. When the outbreak began, there was no vaccine.
Today, the world has a stockpile of half a million doses. This is sufficient for use in preventive vaccination programmes for frontline workers in countries with a history of Ebola, with some kept in reserve as emergency jabs in case of an outbreak.
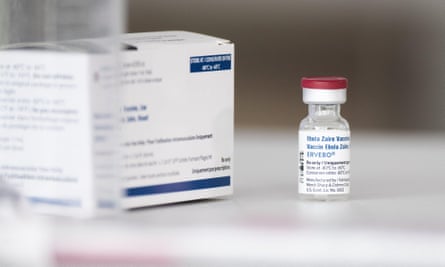
Sierra Leone will this week become the first country to launch a nationwide preventive Ebola vaccination campaign for people at the highest risk. Over three weeks, officials aim to deliver 20,000 doses of Merck’s Ervebo vaccine in a drive that will be repeated every two or three years.
Doses will be offered to healthcare workers, as the country lost 7% of its medical workforce to the 2014-16 outbreak, and also to soldiers and motorbike riders, who provide the main form of transport for many Sierra Leoneans. Also included will be village hunters, who go out in search of bushmeat, since Ebola circulates in animals and can spill over into humans.
The programme is being greeted with optimism as a step towards creating a stronger health system better able to withstand any future outbreaks, but it is clear that memories of 2014 remain raw. “Sometimes, when I’m in my bedroom, I just sit down and cry,” says Kamara.
On 30 October 2014 – five months into Sierra Leone’s outbreak – his mother started to feel ill. The family were reassured by a doctor that she had diabetes and heart problems, not Ebola.
“I said, ‘Oh thank God’,” Kamara remembers. “So all of us – my wife, my father, all of those that [later] died, we started to embrace our mother. I would feed her, use my bare hands to wipe her tears when she was crying. She died on the second day.”
He clutched her body to his chest, he says. Two days later, laboratory results showed that she died from Ebola.
Kamara noticed his own symptoms in early November, 2014: “weakness, diarrhoea, pain all over my back”. He was taken by ambulance to a treatment centre. While he recovered, his relatives were succumbing. His father was taken to a different treatment centre several hours away, where he died.

Two of Kamara’s brothers were brought to his treatment centre. “They died in front of me,” he says. Kamara was released but arrived home to find that his wife, son and stepmother had all died.
Kamara later became a spokesperson for the Sierra Leone Association of Ebola Survivors, and was sent overseas by the government as an ambassador to seek support for survivors. He pushed for support for Ebola orphans, and for widows who in some cases have been forced to turn to sex work.
Today, he says, that support has evaporated. A former professional footballer who once dreamed of playing overseas, Kamara has been left supporting 13 younger relatives. Like many survivors, he says he is unable to find well-paid, regular work. For him, this is because of caring responsibilities. For others, ongoing health issues or stigma play a role.

The cemetery where Kamara’s family is buried is now overgrown with weeds, he says. The government no longer funds offices for the association, and he is not sure what happened to promised social investment funding.
At least 23 health complications have been recorded in Ebola survivors, ranging from eye problems to impotence and deafness. Ministers promised them free healthcare at government hospitals, but Kamara says that patients faced “a lot of stigma” there, and were told they needed to pay for medicines.
He is, however, “100% supportive” of the new vaccination programme. The vaccines are provided from the global stockpile funded by Gavi, the vaccine alliance, which is also providing funding for implementing the campaign. Participants will be part of research into long-term reactions and how the vaccine compares with others given earlier in trials and pilot programmes.

The advent of a new outbreak is “just a matter of time”, says Dr Desmond Maada Kangbai, manager of the Expanded Program on Immunization at the Ministry of Health. “We don’t want to go back to where we were in 2014, when healthcare workers were dying, and patients were being abandoned at treatment centres and hospitals.”
Ebola came to Sierra Leone when an infected person from neighbouring Guinea crossed the border to consult a traditional healer. That herbalist became sick and died, and people who came into contact with the corpse at the funeral carried the virus back to their communities.
after newsletter promotion

Dr Donald Grant, district medical officer in Sierra Leone’s second largest city, Kenema, was studying in the US when the outbreak reached his town. But his wife, also a doctor, was working in the hospital’s maternity ward and caring for their eight-month-old son. “She mentioned she had been attending to a patient [who started] bleeding into the IV line,” Grant recalls.
When blood tests revealed that the patient had Ebola, Grant’s wife had already gone home, so the laboratory called him with the result. When he called his wife to pass it on, she mentioned that their son was breastfeeding – a potential route of transmission. “I was blank,” he says. “Thank God everything went well – she was not infected.”
Many colleagues were less fortunate. Near an isolation ward in Kenema’s hospital compound lies the grave of Dr Sheik Humarr Khan, who was the country’s expert in viral haemorrhagic fever. Khan contracted Ebola and died in August 2014.

Near the hospital compound’s entrance, a monument lists 40 staff who died fighting Ebola, from doctors to security guards. More than a quarter of the healthcare workers who died were based in Kenema.
The vaccine will not be a silver bullet. Gaps in the country’s armour against a new outbreak are evident. Travelling around the country, it is clear that many people still lack reliable access to sanitation and clean water. In the early afternoon, on the road between Kenema and the capital, Freetown, people hold out freshly killed bushmeat to passing cars in the hope of making a sale.
In the border town of Kailahoun, Yusuf Marrah, 30, a herbalist, says he will encourage people who seek his advice to take the vaccine, but that his profession needs more support. During the Ebola outbreak and again during Covid, traditional healers were instructed to stop work, but left without “any source of funds”, he says. And they lack the protective kit given to medical workers.
Without that help, he fears that “they’ll just continue to work as they’ve been working before”.
Dr Mohamed Alex Vandi was district medical officer in Kenema during the 2014 outbreak, and is now deputy director of the National Public Health Agency. The country is in a much better position today, he insists. Community health workers have been issued with tablet computers, enabling real-time reporting and surveillance of suspicious symptoms.
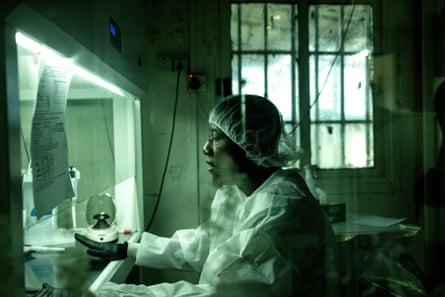
“We don’t take chances,” Vandi says. Lassa fever, another viral haemorrhagic fever (VHF), is endemic in the country and being detected in new areas. Marburg, a third VHF, caused a recent outbreak in Rwanda.
Each week, one or two potential cases of VHF are reported, and tests are carried out for Ebola, Marburg and Lassa, says Vandi. Usually, they are negative.
“If the vaccine was not there, it would have made it very difficult for our workers to be comfortable handling cases they suspect could likely be one of the VHFs,” he says. “Of course, you’re going to take precautions. But at least this will give you some confidence.”
-
This reporting trip was paid for by Gavi, which is funded in part by the Bill and Melinda Gates Foundation, a philanthropic organisation that also contributes funding to support the editorially independent global development section at the Guardian

 2 months ago
47
2 months ago
47













































