When Jake, a businessman in his 50s, first arrives at my therapy practice, it’s obvious that he has some misgivings. Jake’s marriage to Louise is in trouble, and she has insisted he come and see me. “If not for Louise, you wouldn’t be here, would you?” I enquire tentatively. He looks sheepish at first; then emboldened, he gives an emphatic “No.” As is almost always the case, Jake’s wife has registered a problem that has passed him by, and prompted his visit. Over the next few weeks, we sift through a maze of obstacles, and in the end, Jake is full of emotion: “I’m alone in the world, everyone leans on me, there’s no one for me,” he says. “There’s no one to turn to.”
It’s a common pattern, one I’ve seen throughout my 35 years as a psychologist specialising in male mental health. Men make up only 33% of referrals to NHS talking therapies. They don’t come easily, and when they do seek help in a crisis, they can disappear as suddenly as they arrive. Yet male vulnerability is clear – men report lower levels of life satisfaction than women and make up three-quarters of suicides and problems with addiction. But despite the increase in awareness around male mental health, men still tend to think there’s a stigma to speaking with a professional, even though most of those who have tried therapy have a positive experience.
So why are men still so reluctant to talk? Here are the issues I see again and again.
Men are primed for action rather than words
Historically, men’s roles centred on work and provision; women’s on caregiving, looking after the home and raising children. Today, men still tend to be more action-oriented and task-focused. This is partially hardwired – boys tend to lag behind girls in verbal and emotional attunement; women speak more words in an average day.
Action comes before the development of language; it is our mother tongue, and men tend to stick with this early way of communicating, which is shaped both by biology and the social context. When it comes to expressing distress, men find it more difficult to do so verbally. They are far less likely to say they are depressed or anxious; instead, they are prone to acting out when troubled. Without even realising why, they may find themselves driving too fast, getting into altercations, drinking or using pornography when they experience emotional difficulty.
Therapy is ‘feminised’
Women have been more likely to seek professional help in the form of talking therapies, and as a result therapy has developed through the female lens. Services are often “feminised” in design, with an emphasis on talking directly about feelings, which can be uncomfortable for men, who tend to respond better to “shoulder-to-shoulder” conversations than face-to-face discussions.
They often prefer group therapy for its sense of camaraderie and shared experience, allowing connection without being in the spotlight. Coaching and mentoring show promise as male-friendly approaches. I often find this with my patients: you begin by talking about their work setting – an area they feel comfortable discussing – and end up talking about more intimate personal struggles, because going straight into the personal is too threatening. Services working with male veterans combine activity such as walking and talking with traditional talk therapy. The Men’s Sheds Association, which encourages people to come together to make, repair and repurpose, supporting projects in their communities, say that 89% of participants feel less depressed after engaging with it.
Showing vulnerability is risky in a hierarchy
I’m struck by how many men come to see me as a milestone birthday approaches – when they’re 39 or 49, say. Reflecting on a reunion with old friends, one middle-aged patient told me: “What a relief – there was none of the competitiveness that made it so difficult to connect when we were younger. We can all relax now; we’ve got to where we’ve got to in life.” He said he could never have allowed himself to seek therapy earlier: “It would have been like exposing my belly to my adversary without my armour on.”
The drive to strive is deeply encoded in men, and can stop us getting help when we’re down. Showing weakness feels hazardous when your position in the pecking order matters, and yet concealing it ultimately leads to greater fragility. Men are acutely shame-prone when it comes to showing vulnerability, fearing it will lower their status in the eyes of others.
Science helps us make sense of this. Male infants are more emotionally reactive than girls, less able to self-soothe, and more dependent on external regulation from caregivers. Yet we continue to expect boys to be more resilient, to show less emotion. The very infants we encourage to be robust are those most negatively affected when deprived of comfort.
Therapy, which encourages emotional expression, can feel threatening when you’ve been raised to believe that showing your feelings is shameful. I have met many men who struggle with sexual dysfunction but feel unable to talk about it – sometimes avoiding relationships entirely rather than seeking help.
And yet I cannot recall a single younger man who has regretted starting therapy. A safe therapeutic environment allows men to look at the behavioural patterns that limit them – and to begin to let them go.

The age-old go-it-alone mentality
From the 19th-century novel centred on the buccaneer living a solitary existence to the modern cult of the “sigma male” (the online celebration of men who need no one), the legacy of “men going it alone” casts a long shadow. Therapy, by definition, begins with the client admitting they can’t do it all alone.
The single most important thing that makes for a good life is strong, meaningful relationships; they are as important in predicting longevity as being a non-smoker. Yet men find it hard to step away from the powerful and harmful notion that there is safety in being solitary and self-sufficient.
What happens in the therapy room? Gradually, men begin to test out the possibility that connection isn’t weakness but nourishment. The development of an authentic, connected relationship with their therapist proves it.
Emotional claustrophobia
“I don’t think I can keep it up,” says Marcus, referring to his fiancee’s wish to talk about their relationship. “I can do it for a bit, but then we keep going and going and I feel completely overwhelmed.” Later he admits that it makes him feel inadequate.
With men, the expression of strong emotion can often only be tolerated in bitesize chunks. They are often raised to approach difficulties mechanically: identify, act, solve. This is helpful when the problem is practical, but when it is emotional they can become unstuck. Therapy, which requires patience and uncertainty, doesn’t fit this template. It may be necessary to provide men with a practical framework, such as specific techniques to manage symptoms of depression, panic attacks or other problems with anxiety (Why Has Nobody Told Me This Before? by Julie Smith is really useful for this).
They wait until crisis point
Michael had been in a same-sex marriage for almost 30 years when he came to see me. Their sexual relationship was good to begin with, but there hadn’t been much intimacy for the past two decades. It hadn’t occurred to them to seek help, and Michael retreated deeper and deeper into using pornography and talking to strangers online. He felt alone and guilty, acutely depressed and desperate to be released from the prison he had created for himself. Michael’s husband discovered that he was researching methods to take his life and this brought him to my consulting room.
On the whole, men tend to have less patience and want a quick fix. As a result, the threshold for action tends to be higher, and thus men will often allow things to fester and become worse before they seek help. A problem that might have been addressed earlier becomes overwhelming, and can lead to needless despair and suffering.
A shortage of role models
There are exceptions – such as Stormzy, Prince Harry and the footballer Tyrone Mings – but media accounts of men in therapy often emerge when they are in crisis, such as when they go to rehab.
Therapy is framed as a redemptive arc – a tidy solution to adversity. Men often come to therapy expecting immediate results, and need to be helped to let go of the fantasy of a swift remedy, learning instead to turn up, sit with vulnerability and allow progress to unfold in small, unheroic steps.
We rarely see men discussing therapy as routine maintenance, the way we might talk about going to the gym or managing diet. Men are also considerably underrepresented in the psychological professions, including counselling and psychotherapy, which furthers the impression that these services are not suited to the needs of men and boys.
Fear of what they may find
Therapy is about confronting the things we would prefer to avoid. It might uncover long-buried pain, guilt or grief. The fear that the whole structure might collapse if you start pulling on the threads is something everyone must overcome when they seek help, but it is particularly acute in men. They tend to feel deeply ashamed of their suffering, concealing it not just from others but from themselves.
The paradox is that therapy doesn’t strip away strength – it redefines it. It offers a space where control can loosen without consequence, where emotions can be named rather than managed. The real challenge is cultural: masculinity links worth with resilience, while therapy still signals fragility.
If you’re trying to help a man you care about take the first step, offer unpressured side-by-side connection and understanding, not instruction, advice or critique. And if you’re the man hesitating on the threshold, you don’t have to be at crisis point to seek support. It’s not self-indulgent to talk about yourself. Instead it helps you be less self-focused, and to concentrate on the things that really matter, to make good connections with those closest to you.
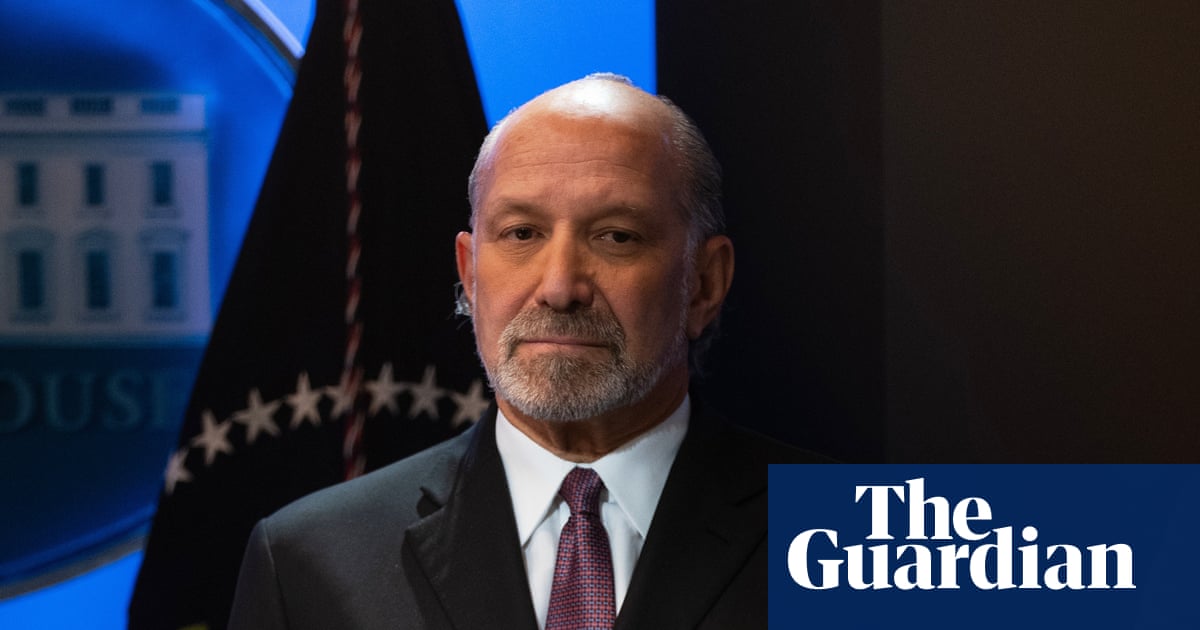
Dr Stephen Blumenthal is a consultant clinical psychologist and psychoanalyst in the NHS and in private practice

 1 month ago
27
1 month ago
27